Abstract
Introduction: Myelofibrosis (MF) is a BCR-ABL1-negative myeloproliferative neoplasm that develops either de novo (primary myelofibrosis; PMF) or secondary to polycythemia vera (post-PV) or essential thrombocythemia (post-ET). JAK2 V617F is the most common somatic driver mutation in MF known to associate with disease progression. Allogeneic hematopoietic cell transplantation (HCT) is the only curative treatment modality for MF. There are limited data regarding the prognostic utility of JAK2 V617F mutation and mosaic chromosomal alterations (mCAs) spanning JAK2 in MF patients undergoing HCT.
Methods: The study included 924 patients undergoing HCT for myelofibrosis (634 PMF, 135 post-PV, and 155 post-ET) between 2000-2016. Pre-HCT peripheral blood samples, clinical and post-HCT data were provided by the Center for International Blood and Marrow Transplant Research (CIBMTR) registry and biorepository. We used PacBio Single Molecule Real-Time (SMRT) sequencing to detect the JAK2 V617F mutation, and Illumina Infinium Global Screening Array-24v1-0 to identify mCAs; this analysis focused on mCAs involving JAK2 (9p24.1). We used the Kaplan-Meier estimator to calculate the probability of overall survival (OS), and the cumulative incidence estimator for relapse/disease progression incidence and non-relapse mortality (NRM), where each was treated as a competing event for the other. Cox proportional hazard models were used for multivariable analyses. Analyses were completed separately by MF disease subtype. Follow up started at date of HCT.
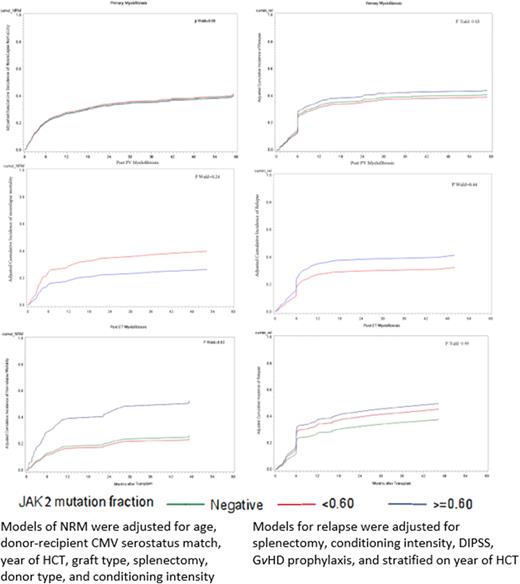
Results:JAK2 V617F mutation was detected in 562 patients (60.8%) with noted expected differences by disease subtype (57.6% of patients with PMF, 97% of post-PV, and 42.6% of post-ET). Almost all patients with mCAs involving JAK2 region were found to be JAK2 V617F mutation-positive (366 out of 374, 97.9%). In JAK2 V617F positive cases, the frequencies of mCA-positive patients per MF subtypes were as follow: 58.08% of PMF, 89.3% of post-PV, and 56.06% of post-ET. The mean allele burden for JAK2 V617F mutation was 57%, 78%, and 60% in PMF, post-PV, and post-ET, respectively. The probabilities of 3-year post-HCT OS were 55% (95% CI=51-58) for PMF, 59% (95% CI=51-67) for post-PV and 59% (51-66) for post-ET. The corresponding 3-year post-HCT cumulative incidences for relapse were 31% (95% CI=28-35), 31% (95% CI=24-40), and 33% (95% CI=26-41); and for NRM were 29% (95% CI=26-33), 25% (95% CI=18-32), and 23% (95% CI=17-30), for PMF, post-PV, and post-ET, respectively.
In PMF, JAK2V617F mutation, JAK2 mCAs, or mutation allele burden were not associated with any of the evaluated HCT outcomes (p>0.05 for all). In post-PV, all four patients without JAK2V617F mutation died in the first 12 months after transplantation. No statistically significant associations between HCT outcomes and JAK2V617F allele burden was noted (p>0.05). For post-ET, patients with high mutation allele burden (³60%) had three-fold excess risk of NRM compared with mutation-negative patients (hazard ratio [HR]=2.9, 95% CI=1.21-6.93, p=0.01). No risk difference was noted between post-ET patients with low allele burden and risk of NRM (HR=0.89, 95% CI=0.34-2.31). No statistically significant association between JAK2V617F mutation status and risk of relapse for high or low mutation allele burden as compared with mutation-negative post ET patients was observed (HR=1.42, p=0.30 in patients with allele burden<60%, and HR= 1.54, p=0.26 for patients with allele burden³60%). JAK2V617F mutation status in post-ET patients was not associated with post HCT OS (HR=1.31, 95% CI=0.78-2.2, p=0.31).
Conclusion: The effect of JAK2V617F mutation on post-HCT outcome differs by myelofibrosis subtypes. HCT outcomes in primary and post-PV myelofibrosis were not associated with JAK2 alterations, but high JAK2V617F mutation allele burden in post-ET was associated with elevated risk of non-relapse mortality but did not translate to a statistically significant survival disadvantage. Our findings suggest that allogeneic HCT for myelofibrosis may alleviate the known negative effect of JAK2V617F mutation in those patients, particularly for primary myelofibrosis and post-PV. It is essential to consider evaluating these findings within the context of other MF driver genes.
Disclosures
Deeg:CSL/Behring: Other: Advisory Board. Gupta:Sierra Oncology: Consultancy; Novartis: Consultancy, Honoraria; Pfizer: Consultancy, Other: Participation on a Data Safety or Advisory board; AbbVie: Consultancy, Other: Participation on a Data Safety or Advisory board; Roche: Other: Participation on a Data Safety or Advisory board; Constellation Pharmaceuticals, Inc., a MorphoSys Company: Consultancy, Honoraria; BMS Celgene: Consultancy, Honoraria, Other: Participation on a Data Safety or Advisory board. Lee:Incyte: Research Funding; AstraZeneca: Research Funding; Amgen: Research Funding; Novartis: Other: Steering Committee; Syndax: Research Funding; Pfizer: Research Funding; Incyte: Research Funding; Kadmon: Consultancy, Honoraria, Research Funding; AstraZeneca: Research Funding; Amgen: Research Funding; Kadmon: Consultancy, Honoraria, Research Funding; Equillium: Consultancy, Honoraria; Mallinckrodt: Consultancy, Honoraria; Pfizer: Research Funding; Syndax: Research Funding; National Marrow Donor Program: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal